Lyme disease tests
Innatoss Laboratories uses antibody tests in a clever way in order to achieve maximum results. With a combination of tests, for example, a lot more insight in a possible Lyme infection can be given. Besides, we are working on the development of a new type of test on the basis of blood cells.
When Lyme disease is suspected, it is first checked whether the well-known red circular inflammation (erythema migrans) is, or was, present. Is this the case, antibiotics are immediately prescribed.
Explanation about antibody tests
When the inflammation is not visible, diagnosis is a bit more troublesome. In most cases, diagnosis is prolonged until the patience experiences the first symptoms, like flulike symptoms, after a tick bite. When a patient has these symptoms, an antibody test is often performed; the so-called ELISA test. Such a test shows whether or not antibodies against specific proteins of the Borrelia bacteria in the blood are present.
Two types of antibodies are tested for; IgM and IgG. In general, the body first produces IgM antibodies, and then, IgG. It takes several weeks before enough antibodies are made to show up in the test. However, every person reacts differently to an infection. In some cases, the antibodies are already present after 3 weeks, while for some people, it takes 10 weeks before the antibodies can be measured.
The ELISA test can separately measure the created IgM and IgG antibodies. Also, the so-called C6-ELISA is executed on a regular basis. This test doesn’t distinguish between the two types of antibodies, and therefore, shows the total amount of both. However, the result of the C6 test doesn’t always correspond with the other ELISA tests. Therefore, three ELISA test should be executed together in the early phase of a possible infection. This is also the basic package that Innatoss uses for the screening of people who are bitten by a tick on a regular basis.
When you have been bitten by a tick more than once, it possible that you already have antibodies. This makes the diagnosis of a new infection more difficult. However, when the results of previous ELISA tests are known, a new infection can easily be recognized. The new test results of the ELISA tests are simply compared to the known profile.
A positive ELISA doesn’t necessarily indicate Lyme disease. It might show an older, already treated infection. This is what makes making the right diagnosis difficult. Therefore, a positive ELISA test is always confirmed with a more sensitive test, the immunoblot, in order to prevent cross-reactivity for example. Cross-reactivity means that the test has detected a different disease than Lyme disease. In some case, a positive IgM result is, for example, caused by gum inflammation.
A doctor will also look at the test result in combination with the clinical observations (symptoms, medical history). The complete picture of the antibodies that are present, such as the 5-in-1 test of Innatoss provides, is an important factor in the diagnosis. However, it is not a diagnosis on its own.
More information on immunoblot
Beside the ELISA, an immunoblot is used. This is a more expensive method that provides more information.
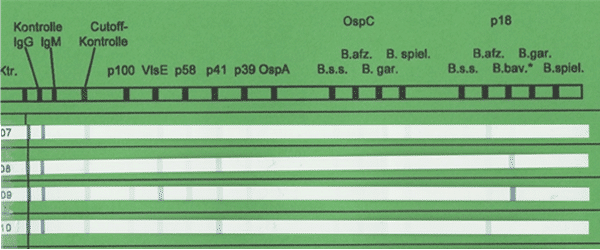
In the classic immunoblot, the “Western Blot”, the proteins of an entire Borrelia bacterium are first separated according to size. These separated proteins are then placed onto a plastic strip. This strip is incubated with the serum sample of the patient, and the antibodies that are present in this sample will bind with these proteins. This reaction is then coloured.
The alternative for this method is the immunoblot with recombinant proteins. This method, which is used more and more often, creates the proteins separately with the help of DNA techniques, and places them on a strip. The remaining part of the procedure is the same as that of the classic immunoblot.
The advantage of the Immunoblot is that you don’t only get to see that antibodies are present, but it also shows against what they are directed. In this way, you don’t only get information on the specific Borrelia strain, but also on the stage of the illness. However, it still goes that what you put in, you will get out. When somebody has antibodies for a Borrelia bacteria of which the proteins are not placed on the strip, these will not be measured. B. spielmanii, for example, is not found by all the test. For this reason, Innatoss works with a combination of Lyme tests in which the different strains are represented.
More information on the ELISA test
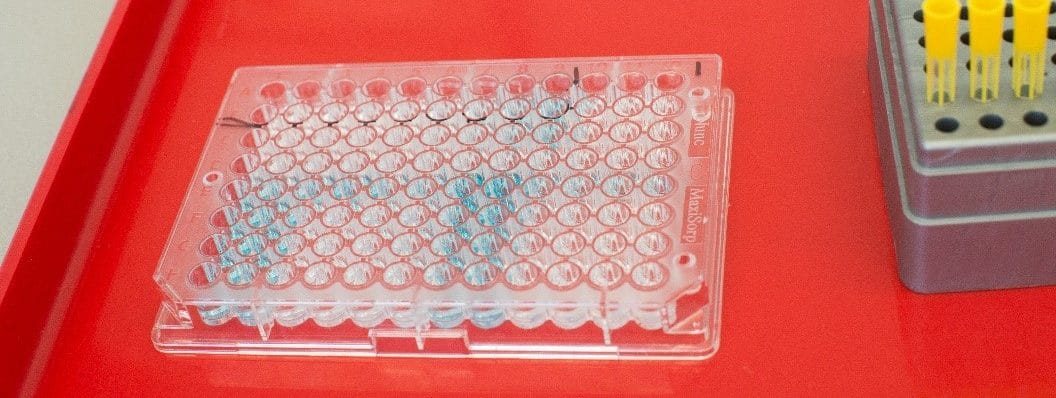
ELISA is short for Enzyme-Linked ImmunoSorbent Assay. Another abbreviation that is used is EIA (Enzyme ImmunoAssay). An ELISA is a method that binds the proteins of a bacteria to the bottom of a 96 well plate. After which, a serum sample of the patient is added. Borrelia antibodies in the serum bind with the corresponding Borrelia proteins in the well. This reaction is made visible by adding different types of reagents. Because of this, a colour is formed. The more colour is shown, the more antibodies were in the sample.
Confusion because of the body’s antibody response
Serological research looks at the formation of antibodies. In case of a Borrelia infection, the IgM antibodies are, generally speaking, formed first, and the production of IgG follows later. However, a number of characteristics of the body’s antibody response can influence this process:
- The Window-phase: The development of antibodies takes some time. For most the patients, it takes 2-8 weeks until the antibodies can be measured. Because of this, the sensitivity of both IgM and IgG is low in the early stage of the infection. For the early symptom EM, this is around 50%, and with neuroborreliosis, this number is around 80%.
- Early successful treatment with antibiotics, like with an EM, can cause limited antibody response. Conformation of the disease after treatment, therefore, is often impossible.
- Serological scar: Once antibodies are formed, they can remain in the body for years. The presence of antibodies, therefore, doesn’t necessarily indicate an active infection.
- Cross-reactivity: Syphilis, viral infections and collagen vascular diseases, like rheumatoid arthritis and SLE, can cause a cross-reactivity in antibody tests, especially when testing for IgM antibodies. This causes a false positive result.
- Seronegative Lyme disease: Not all patient react with an antibody response. Therefore, these infections aren’t detected when only antibody tests are used. The experts don’t see eye to eye on this matter. However, it should be taken into account that the Borrelia bacteria knows how to avoid the immune system. When a patient is seronegative and does have the symptoms that are characteristic for Lyme disease, an infection might be present.
More certainty is possible
- Repetition: This is helpful for multiple reasons. Repetition of the tests helps to cover the Window-phase, and reduces the chance of a false negative result. What’s more, a follow-up test can separate a recent infection from a serological scar: increasing values indicate a recent infection. In case of a serological scar, an increase will not take place. The Lyme Basic test with 3 ELISA tests forms a good follow-up tests, without directly using the expensive immunoblots.
- Multiple tests in parallel: At Innatoss, tests of different producers are executed on the same sample in order to get more certainty about a possible infection. This is slightly more expensive; however, a false negative result will cost a lot more in the end. A clear exclusion of Lyme disease often also prevents a repetition of steps. By immediately testing for multiple bacterial strains, an answer can be given fast or excluded Lyme disease.
Have a look in our online shop for more information on the tests that Innatoss Laboratories offers.
Confusion because of the use of different tests
The technical reproduction of the ELISA’s and immunoblots is good. The repetition of the same samples or a new sample of the same patient will present the same results. In technical respect, these tests are very reliable. Then, how did the idea arise that serological research is unreliable?
- Producers use different combinations of the Borrelia proteins and use different cut-off values.
- Multiple Borrelia strains, which have different proteins, exist. When someone produces antibodies against B. afzelii, these will bind hardly or not at all with the proteins of the B. garinii bacteria during an antibody test.
- Laboratories in the Netherlands use tests of different producers and in different combinations.
Because of the aforementioned, contradictory results arise. A patient can, for example, get a negative result in one laboratory, while in another, the results are positive. This causes a lot of confusion for both the general practitioner and the patient.